In Japan, aspiration pneumonia has become a major issue as the population ages.
This blog has previously introduced tools and techniques that support oral intake—such as thickening agents, the K-spoon, and capsaicin.
At the same time, some people choose enteral nutrition (via a gastrostomy tube or a nasogastric tube) due to illness or other reasons.
In Japan, life-sustaining treatments have traditionally been emphasized, so enteral nutrition has been widely used.
In recent years, however, there has been more discussion about its necessity and ethical considerations, and choices appear to be shifting.
Although I have personal views on the pros and cons, as a nurse I focus on making enteral nutrition as safe and comfortable as possible in daily practice.
This article looks at semisolid enteral formulas used for tube feeding.
Liquid formulas are the mainstream, but in some cases a semisolid option is chosen.
Here, I explain the basics of enteral nutrition and semisolid formulas, and I also introduce a related patent.
Note: This article is based on my own investigation. It does not guarantee accuracy.
Please make any purchase or use decisions at your own discretion.
Some links in my articles may be affiliate links (PR).
When Eating Becomes Difficult
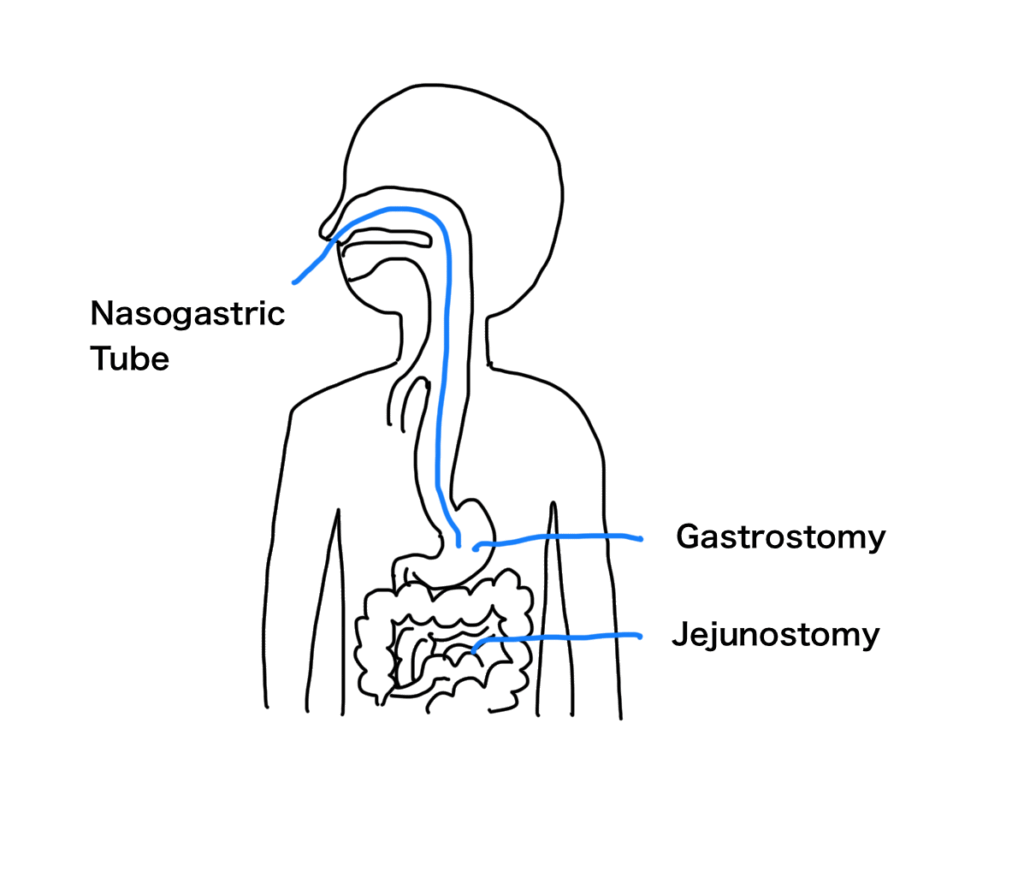
Enteral nutrition delivers nutrients into the intestine through a nasogastric tube (NG tube) or a gastrostomy tube (G-tube). In clinical settings it is often called “tube feeding.”
When illness or aging makes oral intake difficult, patients and families select from the options below after receiving an explanation from the physician:
- Tube feeding (gastrostomy, nasogastric tube, jejunostomy, etc.)
- Central venous nutrition (parenteral nutrition via a catheter placed in a central vein; “TPN”)
- Peripheral IV (short-term infusion or drug administration via a peripheral vein; high-calorie infusions are not possible)
I will not go into detail about IV therapy here, and each method has advantages and disadvantages.
When the GI tract can be used, enteral nutrition is generally preferred.
In my experience, careful discussion about whether nutrition support is truly necessary has increased. At home and in long-term care settings, some people choose to forgo interventions, including IV fluids.
As a nurse, I value supporting patients and families to make informed choices that reflect their wishes and medical appropriateness.
Benefits of Enteral Nutrition
- Helps maintain digestive and immune function
The GI tract contributes to both digestion and immunity. Because enteral nutrition uses a route close to normal oral intake, it can help preserve intestinal function.
Common Problems
- Aspiration pneumonia
If gastric contents reflux and pass the larynx into the airway, aspiration pneumonia can occur.
- Diarrhea
Many formulas have high osmolarity. If a concentrated formula enters the small intestine rapidly, water is drawn into the intestinal lumen and diarrhea may result (explained later).
- Risk of pressure injury
Long infusion times and prolonged positioning can increase the risk of pressure injuries.
Features of Semisolid Nutrition
A semisolid enteral formula is one strategy to reduce some tube-feeding problems.
It has a thick, pudding-like consistency—between liquid and solid.
Potential benefits include:
- Less reflux (higher viscosity flows more slowly)
- Less diarrhea (slower delivery to the intestine and gentler absorption)
- Shorter administration time, which may reduce discomfort and the risk of pressure injuries
There are two main types:
- Semisolid before administration (often used with a wider gastrostomy tube)
- Liquid on administration that gels in the stomach (can be used with a thinner nasogastric tube)
Both types seek to balance usability with nutritional quality.
In this article I focus on formulas that are semisolid before administration and introduce a related patent.
Practice of Enteral Nutrition
Semisolid formulas are available as foods on the market, commonly in pouches of about 120–400 g.
Some products are also available by prescription with insurance coverage.
In many facilities and hospitals, adopted products are pre-determined. When patients transition home, insurance-covered formulas are often chosen to reduce cost.
Syringes, tubes, and pressure bags are also used for administration.
In home care, visiting nurses provide instruction to family caregivers as needed.
Patent on Semisolid Nutrition
- Publication No.: JP 2022-154097 A
- Publication date: October 13, 2022
- Title: Semisolid Nutritional Composition
- Applicant: Terumo Corporation
Conventional Problems
Liquid formulas can present the following issues:
- Reflux and aspiration
- Dumping (rapid gastric emptying) and diarrhea
- Long administration time and increased risk of pressure injury
Contributing factors include low viscosity, high osmolarity, and long infusion times.
Traditionally, agar or thickening polysaccharides (hydrocolloids such as pectin, alginate, or xanthan) have been added to raise viscosity.
However, adding dietary fiber may raise viscosity too much, requiring excessive force to infuse and increasing caregiver burden.
Outline of the Solution
This patent balances agar, high-methoxyl (HM) pectin, and dietary fiber to achieve a texture that holds its shape yet still flows.
Below are the roles of each component.
Agar
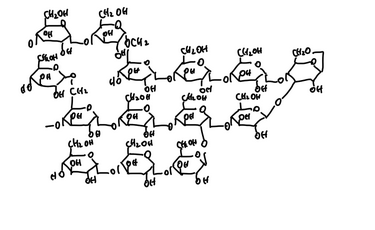
Agar consists mainly of agarose, a long, chain-like polysaccharide.
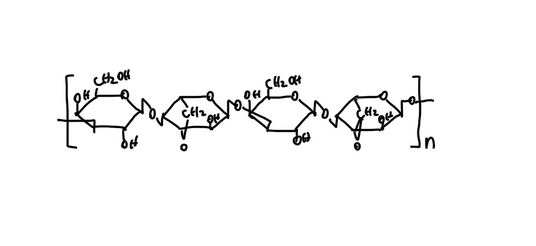
When agar is dissolved in hot water, the chains of agarose molecules are dispersed in a random coil state.
As the solution cools, the chains align and form many double-helix structures.
These helices then gather together, creating a three-dimensional network structure.
Water becomes trapped inside this network, resulting in a firm gel.
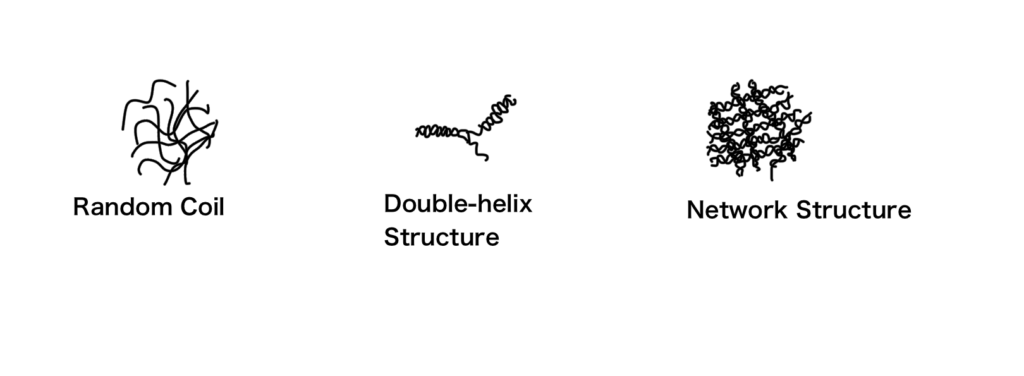
Heating disperses the chains in water; cooling forms double helices and then a three-dimensional network that traps water, creating a gel.
Agar gels hold their shape well at room temperature but can become too firm and resist flow.
Therefore, the patent limits agar to 0.1–0.7% to maintain shape without becoming too hard.
HM Pectin
HM pectin (degree of esterification ≥50%) forms gels under acidic and high-sugar conditions, creating a relatively soft network.
When force is applied, the network can temporarily relax, allowing flow.
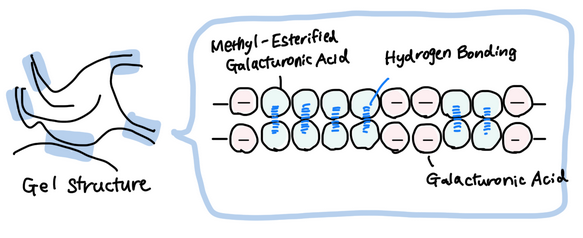
A more detailed explanation of the gelation mechanism of HM pectin can be found in this article.
The patent examples maintain pH 3.0–4.5 and add 0.3–1% HM pectin.
Combining agar’s firm framework with HM pectin’s flexibility results in a gel that is neither too hard nor too soft.
Dietary Fiber
Dietary fiber supports bowel function but can raise viscosity depending on type and molecular weight.
The reason is that dietary fiber consists of long chain molecules that hold a lot of water, entangle with each other, and form a network through hydrogen bonds involving –OH groups.
The patent controls viscosity by:
- Selecting low-molecular-weight fiber (≈1,000–25,000)
- Using fiber with ≤10 mPa·s viscosity (5% solution)
- Setting the addition at 1–5%
This balances the benefits of fiber with ease of infusion.
Osmolarity
Diarrhea often involves osmotic mechanisms. When a concentrated formula enters the intestine, water moves into the intestinal lumen and peristalsis increases.
The patent designs osmolarity at 400–500 mOsm/L and also manages osmolarity through the choice of fiber (smaller molecules increase the number of particles and tend to raise osmolarity).
(Note: The patent specifies osmolarity in mOsm/L; clinical nutrition texts often use osmolality in mOsm/kg.)
pH
pH is key for HM pectin gelation. Maintaining pH 3.0–4.5 reduces electrostatic repulsion between pectin chains and stabilizes the network.
Closing Thoughts
In my experience, changing social values and reimbursement policies may gradually decrease the number of people who choose tube feeding.
Even so, many people still benefit from these formulas.
Industry news has also reported a product from Morinaga that gels in the stomach (“Wanoka”), suggesting ongoing demand.
To reduce complications and burden, it is important to understand formulation design and apply it appropriately.
This time I covered products that are semisolid before administration.
Next time I will discuss formulas that are liquid on administration and become semisolid in the stomach.
I also write technical articles on medical and care materials, and support market entry projects by combining nursing experience with patent knowledge.
Please feel free to contact me via the blog’s form.
Disclaimer: This article is for reference only and does not guarantee accuracy. Please make purchase and use decisions at your own responsibility.
References
Shokuhin Labo. https://shokulab.unitecfoods.co.jp/article/detail13/
Ina Shokuhin Kogyo Co., Ltd. https://www.kantenpp.co.jp/kanten/about
Tatoorui.com. https://www.tatourui.com/about/type/09_agar.html
AIIR Gijutsu Kenkyujo. https://engineer-education.com/dietary-fiber/#3-1
Sakai Tateo, Kaibou Seirigaku, Igaku Shoin, 2010
McMurry, John. Organic Chemistry, 8th ed., Cengage Learning, 2012.
Urabe Yoshitsune, Kagaku no Shin Kenkyu, Sanseido, 2019


