Have you ever experienced swelling in your legs after a long day of work?
Edema, commonly known as swelling, is not only uncomfortable in daily life but also an important issue in nursing and elder care settings.
Recently, I joined a training session that covered lymphatic drainage techniques and compression bandaging.
It gave me an opportunity to revisit the mechanisms behind edema and the innovations being developed to address it.
In this article, I will walk you through what edema is and why it happens, how blood and lymphatic circulation are involved, and what impact edema can have on health and daily life.
I will then explain the mechanisms by which compression helps improve edema and finally introduce a Japanese patent that proposes an innovative design for compression stockings.
Disclaimer: This article is based on my own research and professional perspective.
It does not guarantee the accuracy of the information provided.
Decisions regarding purchase or use of products should be made at your own responsibility. Some links in this article may contain affiliate programs (PR).
What is Edema?
Edema occurs when the balance of body fluids is disrupted and excess fluid accumulates in the tissues.
While it may appear as temporary swelling in the legs due to gravity, it can also result from underlying conditions such as heart, kidney, or liver disorders.
Circulation and Edema
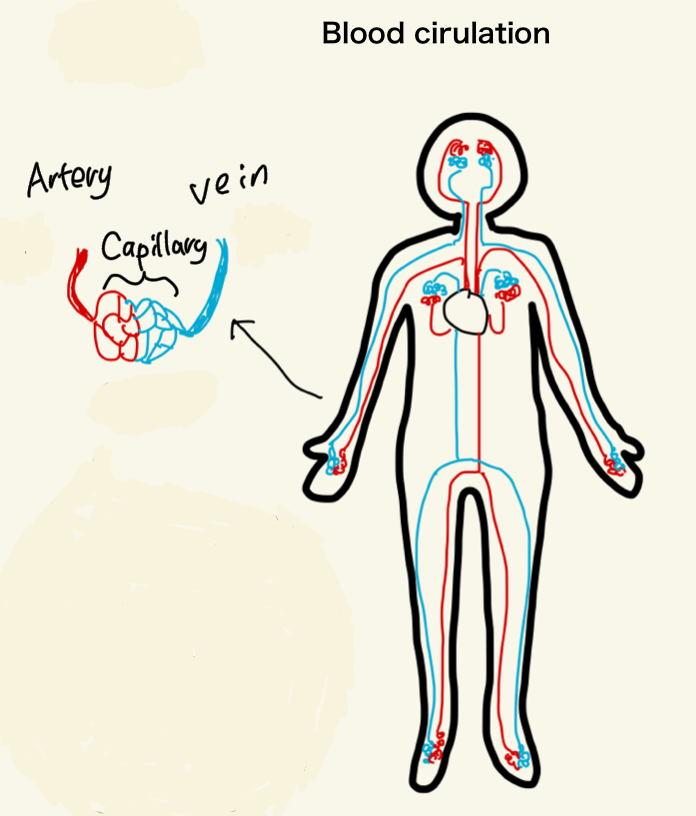
Blood Circulation
Blood carries oxygen and nutrients through arteries to capillaries, and then returns carbon dioxide and waste products via the veins.
While the heart pushes blood forward, veins lack their own pumping mechanism and easily stagnate.
To compensate, the body relies on:
- Muscle pump function: muscles such as the calf compress veins and push blood upward.
- Venous valves: prevent blood from flowing backward.
When people remain seated or standing for long periods, muscle pump activity decreases and swelling in the legs can develop.
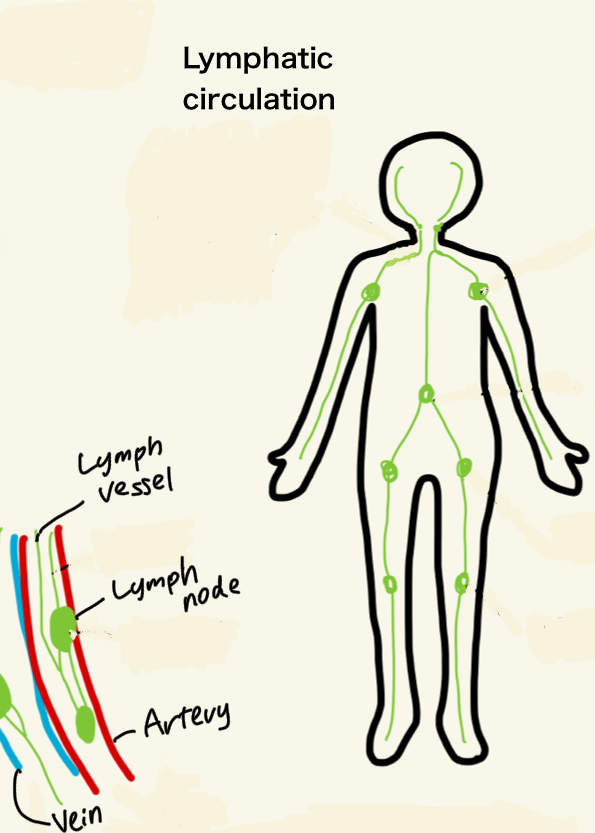
Lymphatic Circulation
When blood passes through capillaries, part of the plasma seeps out into the tissues as interstitial fluid.
Most of this fluid (about 90%) returns to the veins, but the remainder enters the lymphatic vessels.
Lymphatic flow does more than simply return fluid alongside the veins.
Before reaching the bloodstream, it passes through lymph nodes, where immune cells inspect and process foreign matter such as bacteria, viruses, or even cancer cells.
In this way, the lymphatic system functions as an important filter and defense network, not only for fluid balance but also for immunity.
Finally, lymph fluid rejoins the bloodstream via the subclavian veins.
Since the lymphatic system lacks a heart-like pump, circulation depends on muscle movement and the contraction of lymphatic vessels themselves.
Prolonged immobility or lack of exercise slows lymphatic flow, leading to swelling and sometimes reduced immune function.
Types and Causes of Edema
- Localized edema: occurs when circulation is obstructed in a specific area.
Examples include venous insufficiency, post-surgical lymphedema, or swelling from inflammation. - Systemic edema: results from organ dysfunction, such as kidney disease, heart failure, or liver cirrhosis, as well as malnutrition or endocrine disorders.
Impact of Edema
Beyond the visible swelling and heaviness, edema can cause coldness, nighttime urination, and—in cases of lymphedema—skin thickening and higher infection risk.
Severe edema in the limbs can impair mobility, and when fluid accumulates in the lungs, breathing difficulties may occur.
Swelling should not be dismissed as merely cosmetic; it can be a warning sign of serious illness.
Mechanisms of Edema Improvement
Prevention and Management in Clinical Care
In hospitals, prolonged immobility raises the risk of deep vein thrombosis (DVT).
DVT can become life-threatening if a clot travels to the lungs.
To prevent this, medical staff assess risk and may apply elastic stockings (compression stockings) or compression bandages.
In post-surgical patients unable to move their legs, intermittent pneumatic compression devices (often called “foot pumps”) are used.
For lymphedema, doctors may prescribe manual lymphatic drainage performed by trained therapists.
For everyday swelling, common measures include elevating the legs, gentle massage, and wearing compression socks.
How Compression Works
Leg elevation and massage are intuitive methods.
But why does continuous external compression, such as from stockings or bandages, work so effectively?
Think of water flowing through a garden hose.
When the diameter of the hose is gently narrowed, the same amount of water must flow faster.
This is explained by the principle
flow = cross-sectional area × velocity.
The same happens in veins and lymphatic vessels:
- The lumen narrows slightly under compression.
- Flow velocity increases.
- Stagnation is reduced.
At the same time, fluid dynamics follow Bernoulli’s principle.
As velocity increases, static pressure decreases.
Lower pressure on the vessel walls means less fluid leaks into surrounding tissues.
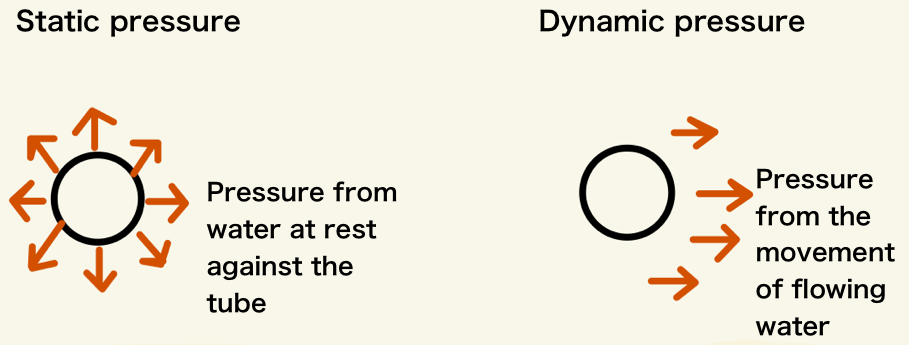
Thus, compression both enhances fluid return and reduces leakage into tissues.
This dual effect makes compression therapy a powerful tool in managing edema.
Proper application is essential: compression must be firm enough to be effective but evenly distributed to avoid obstructing flow or creating areas of pooling.
Patent Example: Compression Stockings
One Japanese patent (JP2023-168867) illustrates how innovation addresses real-world challenges.
Note: The above products are affiliate links for the Japanese market (Amazon Japan, Rakuten).
Conventional Challenges
Traditional medical compression stockings apply strong pressure, but they are difficult to put on and remove, especially for older adults or people with limited hand strength.
Caregivers also find them time-consuming to assist with.
Features of the Invention
- Slit with zipper: allows easy donning and doffing without excessive effort.
- Elastic band inside slit: prevents distortion of shape when the slit is open.
- Heel opening: There is an opening at the heel that creates a catch point, which prevents the stocking fabric from being pulled upward together with the zipper.
In addition, the position of this opening is designed to avoid alignment with the extension line of the zipper.
As a result, when the zipper is pulled up, the load is distributed in three directions—along the extension line, toward the instep, and toward the edge of the heel—allowing the stocking to be raised smoothly.
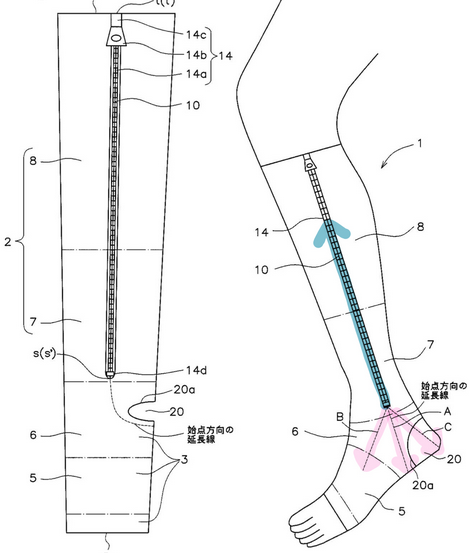
(Figure prepared with reference to JP2023-168867, with minimal elements highlighted and annotated)
- Graduated compression: higher pressure at the ankle, lower pressure toward the calf, promoting venous return.
Slightly higher pressure under the arch supports comfortable walking. - Open-toe design: accommodates different foot shapes and reduces burden.
Potential for Home Care
With healthcare shifting from hospitals to homes, products that are easier to use for both patients and caregivers are increasingly important.
This invention suggests one way compression technology can adapt to meet these needs.
Of course, as with all medical devices, use must follow medical guidance, particularly for patients with vascular, neurological, or skin conditions.
I write technical articles on medical and care materials, and support market entry projects by combining nursing experience with patent knowledge.
Please feel free to contact me via the blog’s form.
Disclaimer: This article is provided for informational purposes only and does not guarantee accuracy.
Product purchases or use should be made at your own judgment and responsibility.
References
- Takeo Sakai (2010), Anatomy and Physiology, Igaku-Shoin
- Japanese Patent Application JP2023-168867, “Elastic Stockings”
- Lymphedema Network Japan: https://lymnet.jp


