When people think of injection pain, they often imagine the initial prick when the needle enters the skin.
In reality, pain can occur at several stages: when inserting the needle, advancing it, injecting the medication, and finally removing it.
As a nurse, I have seen how patients often tense up during injections. That’s why I always try to insert the needle smoothly and confidently, keep my hand steady, and speak in a calm, reassuring tone.
Pain reduction doesn’t depend on technique alone. The design of the needle itself can also make a difference.
While many people encounter injections only during vaccinations or blood tests, others such as people with diabetes may need to inject themselves multiple times a day.
For them, injection pain is more than a brief discomfort. It can affect their quality of life.
In this article, I’ll explore the causes of injection pain and introduce a friction-reducing needle coating developed by Terumo, as described in one of their patents.
Injection Pain
Let’s take a closer look at the different steps of an injection and how pain can occur at each point.
1. When inserting the needle
To begin, the needle is placed against the skin at the intended injection site.
Naturally, the needle doesn’t penetrate with a gentle touch alone.
This is due to the skin’s natural elasticity and structural resistance.
As more force is applied, the needle tip begins to break through the skin.
At this point, friction occurs between the needle’s surface and the skin, making it harder for the needle to advance smoothly.
The pain felt during this step is primarily due to nociceptors (pain receptors) located in the skin.
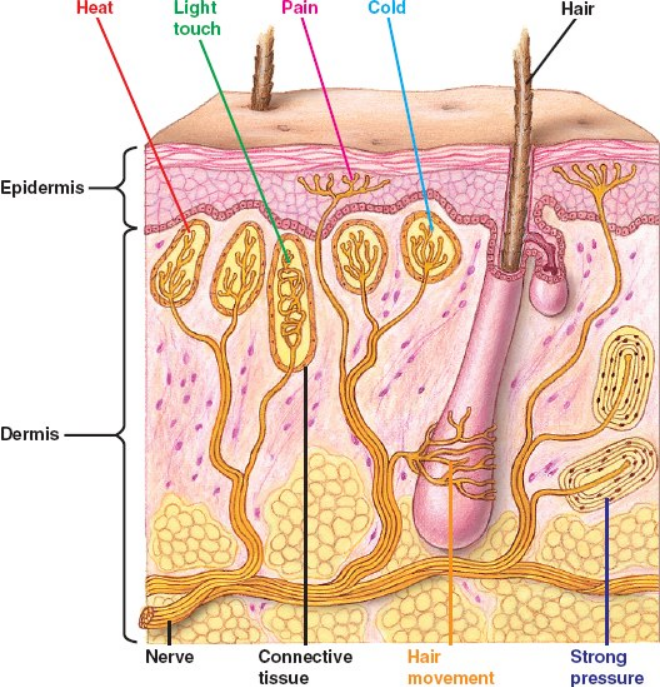
Source:https://www.bio1152.nicerweb.net/Locked/media/ch49/nociceptors.html
2. When advancing the needle
As the needle moves deeper into the tissue, friction continues between its surface and the surrounding tissue.
This movement stretches and deforms the tissue, pulling cells along in the direction of the needle’s path.
In some cases, this mechanical stress can cause cellular deformation or even rupture.
When cells are damaged, they may release substances such as histamine, which can heighten the sensation of pain.
3. When injecting the medication
The pain from an injection isn’t just caused by the needle itself.
Patients may also feel discomfort during the actual injection of the medication.
Many people report that during a flu shot, the injection itself hurts more than the moment the needle pierces the skin.
This pain is often caused by differences in pH and osmotic pressure between the medication and the body fluids.
4.When removing the needle
Even as the needle is withdrawn, friction still occurs between its surface and the tissue.
As with insertion, this can lead to slight discomfort or a dull ache.
Although brief, this sensation adds to the overall pain experience of the injection process.
How to Reduce Injection Pain
As we’ve seen, much of the pain experienced during an injection comes from the resistance encountered when the needle pierces and advances through the skin and tissue.
In other words, reducing that resistance also reduces the force needed to insert the needle, which in turn can help ease the pain.
Here are some common strategies used to minimize this kind of pain:
• Stretching the skin tightly
→ This helps reduce the skin’s elastic recoil and makes it easier for the needle to penetrate.
• Sharpening the needle tip
→ A sharper tip can cut through the skin’s structural resistance more easily.
• Applying a surface coating to the needle
→ A coating reduces friction between the needle and the skin, helping the needle glide in more smoothly.
• Using a thinner needle
→ A smaller diameter reduces stimulation of pain receptors, which can lessen discomfort.
Here, we’ll take a closer look at a patented needle coating designed to reduce friction and ease injection pain.
A Coating Agent Patent That Eases Injection Pain
International Publication No.: WO2018/123276
Publication Date: July 5, 2018
Japanese Publication Date: November 7, 2019
Title of Invention: Coating Agent and Medical Device Surface-Treated with the Coating Agent
This patent focuses on a special coating agent applied to injection needles, aimed at reducing the pain and discomfort people often feel during injections.
In general, “coating” refers to covering the surface of an object with a thin film.
It might seem like simply making the surface smoother would help the needle slide in more easily.
That said, this invention goes a step further and introduces several key innovations beyond just improving slipperiness.
The Problem with Conventional Coatings
As you may know, one major cause of pain during injection is the friction that occurs when the needle pierces the skin.
To reduce this friction, silicone-based coatings have commonly been used.
While these do help to some extent, there are still some drawbacks:
• The pain is not completely eliminated.
• Repeated puncturing can cause the coating to peel off.
Now, when we talk about “repeated puncturing,” this doesn’t mean using the same needle multiple times on a patient.
Rather, in clinical practice, nurses often need to draw medication from a vial or ampule using a syringe.
This often involves puncturing a rubber stopper or brushing against the sharp glass edge of an ampule—both of which can damage the coating.
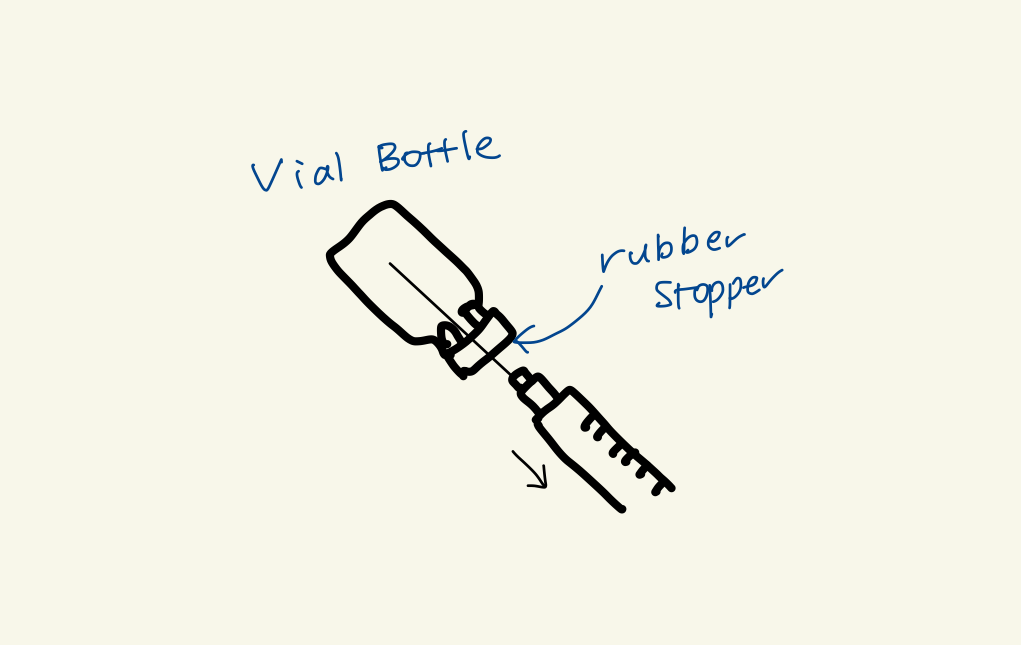
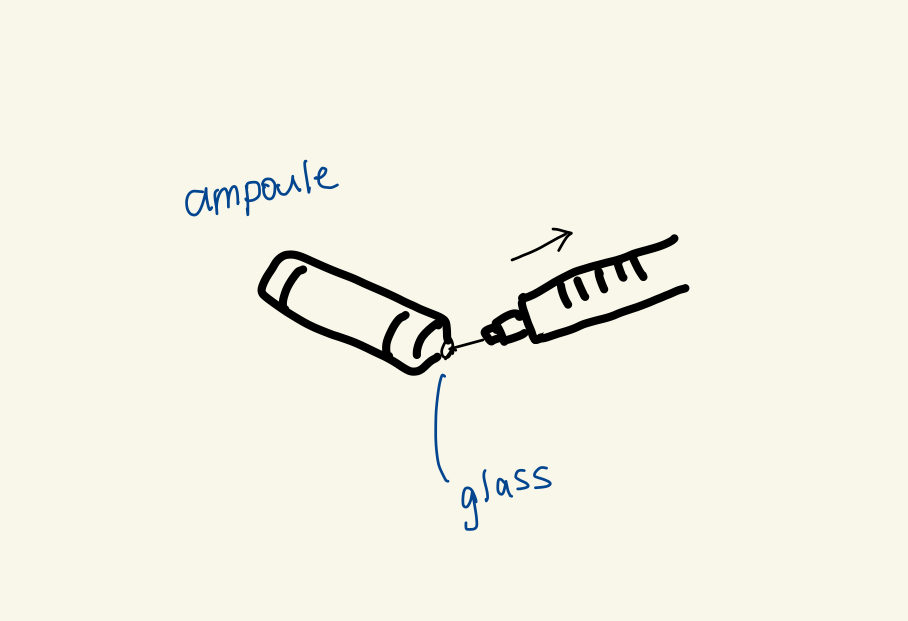
From my own experience, I’ve noticed that when the coating peels off, the needle suddenly feels dull and harder to insert.
To prevent this, we usually replace the needles used for drawing medication with a fresh needle for injection.
But depending on the situation, replacing the needle may not always be feasible.
Even when we change needles, the coating may have already peeled off.
If that happens, it could mix into the medication, which is definitely something to avoid.
This patent proposes a solution in the form of a coating that combines both low friction (reducing insertion resistance) and strong durability (less likely to peel off).
The Solution
This coating agent uses a blend of different types of polyorganosiloxanes (silicones) to reduce friction while also improving durability.
What Is Polyorganosiloxane?
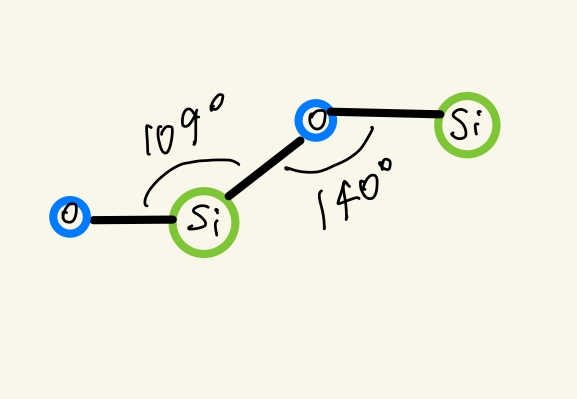
Also known as silicone, polyorganosiloxane is a polymer with a backbone made of siloxane bonds (–Si–O–).
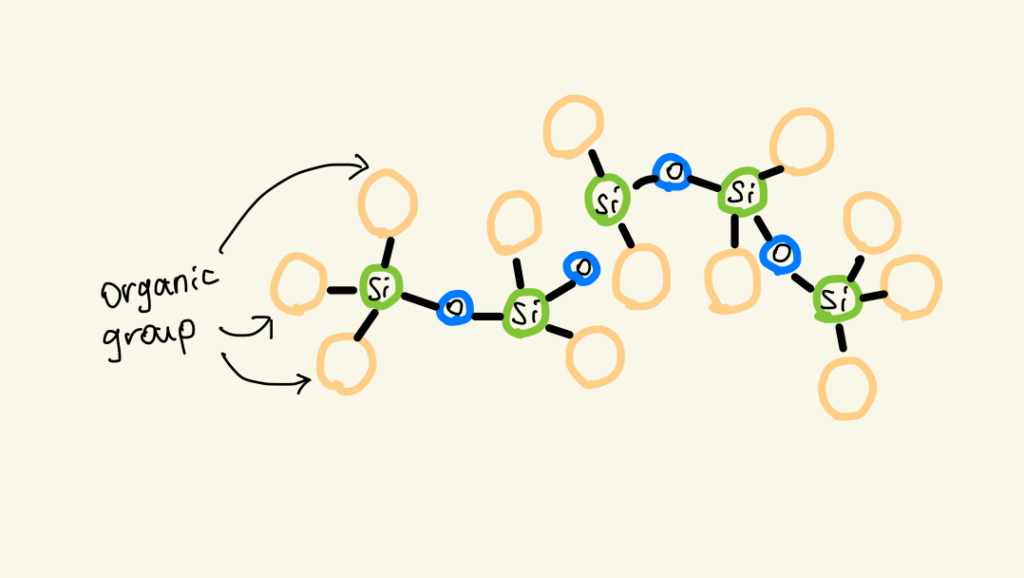
Attached to this backbone are various organic side groups, such as methyl or amino groups.
The Si–O bond is quite strong because of the large difference in electronegativity between silicon and oxygen.
This makes the material chemically stable and resistant to breakdown from heat or oxidation.
Siloxane bonds also form wide bond angles, and since the side chains usually aren’t bulky, the polymer chains are flexible and mobile.
Thanks to these features, silicones are widely used in medical materials and cosmetics.
The Four Types of Polyorganosiloxanes Used in This Coating
The coating described in the patent uses the following four types of polyorganosiloxanes:
① High-polymerized polyorganosiloxane
Large molecules (molecular weight: 250,000–800,000) that form long chains with hydrocarbon side groups.
② Low-polymerized polyorganosiloxane
Shorter chain molecules (molecular weight: 2,000–4,000) with similar structures.
③ Amino group-containing polyorganosiloxane
Polymers with amino groups (–NH₂) on their side chains.
④ Hydroxyl group-containing polyorganosiloxane
Polymers with hydroxyl groups (–OH) on their side chains.
Among these, a combination of:
① + ② + ③ or ④
is used to create a coating that offers both excellent lubricity and durability.
What Each Component Contributes
●Strong Adhesion & Durability
The amino or hydroxyl groups in ③ or ④ chemically bond with hydroxyl groups on the metal surface of the needle. These metal hydroxyl groups form naturally when the surface oxidizes and reacts with moisture in the air.
This bonding helps the coating adhere tightly to the needle surface, making it much less likely to peel off.
●Strong Film Formation
The amino or hydroxyl groups in ③ or ④ also form hydrogen bonds and electrostatic interactions with other silicone molecules, creating a mesh-like molecular network that holds the film together more tightly.
This thin film, or coating layer, adheres to the needle’s surface and retains its structure.
●Friction-Responsive Lubrication
• When light friction is applied:
A polymer with a low degree of polymerization (short, low-molecular-weight polymer; polymer ②) is loosely held within the coating and seeps to the surface, reducing friction.
• When stronger friction is applied:
A polymer with a high degree of polymerization (long, high-molecular-weight polymer; polymer ①), which is more entangled in the network, is pushed to the surface and adds further lubrication.
This mechanism is similar to pressing on a sponge soaked with water—liquid slowly seeps out in response to pressure. In this case, it’s not actual liquid but flexible polymer chains that ooze out to improve slipperiness.
Alternative Approaches to Less Painful Injections
Reducing the pain caused by injection needles isn’t limited to coating technologies.
Here are two other fascinating innovations that take a different approach.
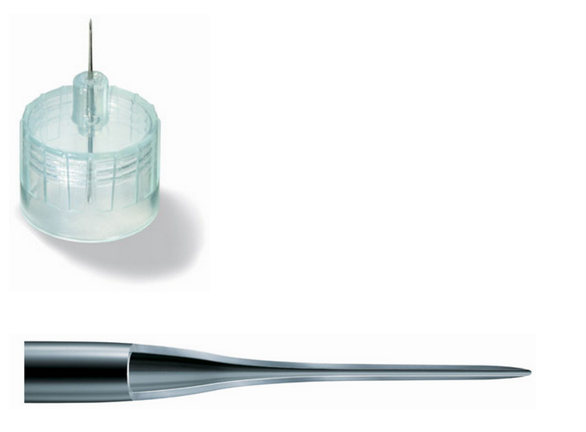
● Ultra-fine Needle: Nanopass (Okano Industrial × Terumo)
Traditional needles are made by rolling a metal sheet into a tube and then drawing it out to make it thinner.
That said, there’s a limit to how fine needles can be made using this method.
To overcome this, a new technique was developed using press molding(a process where a flat sheet of metal is shaped by pressing it into a mold).
This allows the needle to be formed directly from the metal sheet, making it possible to manufacture extremely thin needles efficiently and at scale.
What’s more, the needle has a tapered structure, gradually narrowing from the base to the tip.
This reduces resistance when liquid flows through the needle, making injections smoother.
What’s truly impressive is that this innovative needle was developed by Okano Industrial, a small factory in Japan.
Source:https://www.business-plus.net/console/special/1006/141901.shtml
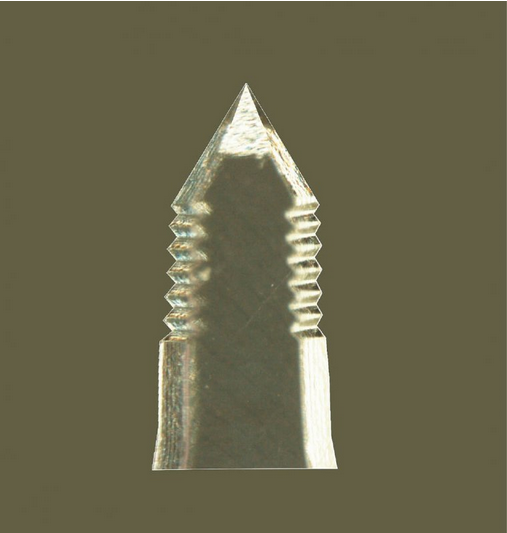
● A Resin Needle Inspired by Mosquitoes (Lightnix)
Researchers were inspired by the mosquito’s needle-like mouthpart.
It has tiny serrations that help reduce pain.
This unique structure was adapted for use in injection needles.
In addition, the needle is made from a soft, plant-based resin that causes less discomfort than traditional metal needles.
Advanced polishing techniques are also used to create an ultrasmooth surface, eliminating even the tiniest irregularities.
Source: https://ab.jcci.or.jp/article/18293
Cost Comparison
| Product Name | Intended Use | Price (Per Unit, Approx.) |
|---|---|---|
| Terumo Subcutaneous Injection Needle 27G (NN-2719S) | Vaccination, subcutaneous injection | Approx. ¥3–14 |
| Terumo Nanopass 34G | Insulin injection | Approx. ¥30–60 |
| Lightnix Resin Needle | General use including vaccines | Approx. ¥50–100 |
Since both Nanopass and Lightnix resin needles are designed for subcutaneous injections, we chose Terumo’s 27G metal needle for subcutaneous use as a reference for comparison.
(It’s unclear whether the coating technology discussed in the article is used in this product.)
Needles that incorporate specialized technologies tend to be priced higher than standard ones.
Future Demand in Japan
In Japan, there is a clear shift toward separating medical roles—hospitals focus on acute care, while long-term recovery and daily care are increasingly managed at home.
Patients are often discharged soon after treatment, and the expectation is that ongoing care will continue outside the hospital.
As the number of hospitals declines and healthcare resources become more limited, the scope of treatments carried out in home care is expected to grow.
Currently, needles used at home are mainly for chronic care: self-injection of insulin, blood glucose monitoring, vaccinations or blood draws during home visits, or infusion via central venous ports.
But looking ahead, it’s likely that more therapeutic interventions will be completed entirely in home settings.
This will naturally change what’s expected of injection devices, such as:
- Long-acting formulations that only need to be injected weekly or monthly
- Devices that patients or family members can handle with ease
- An increase in home infusion therapy → devices must be safe and reliable even when handled by a single healthcare provider
In short, demand is expected to grow for safer and simpler injection tools that anyone can use with confidence.
Closing Thoughts
As healthcare continues to shift toward home-based settings, the demand for injection tools that minimize pain and are easy to use will only grow stronger.
That’s why I want to help ensure that the right technologies reach the people who truly need them, such as patients and caregivers.
With clinical experience in nursing and a focus on medical device patents, I aim to support the spread of practical innovations that make a real difference in home care.
If you’re interested in connecting or would like to share information about innovative products, feel free to get in touch.
References
- WO2018/123276, Coating agent and medical instrument surface-treated with said coating agent, International Publication Date: July 5, 2018; Publication Date: November 7, 2019. Terumo Corporation.
- JP2007-38021A (P2007-38021A), Metal Injection Needle, Japanese Patent Publication Date: February 15, 2007. Terumo Corporation and Okano Industrial Co., Ltd.
- JP2006-297141A (P2006-297141A), Medical Needle and Medical Device, Japanese Patent Publication Date: November 2, 2006. Lightnix Co., Ltd.
- Yasuo Okaneya (Ed.), Byouki ga Mieru Vol.14: Dermatology, First Edition, Medic Media Co., Ltd., 2020.
- Yasuo Negishi, The Japanese Factory Power the World Respects, Discover Twenty One, Inc., 2010.
- Lightnix Co., Ltd. Website: https://www.lightnix.jp
- Lightnix Product Catalog (2018): https://www.lightnix.jp/wp-content/uploads/2018/12/catalog_201812.pdf
- Momentive Performance Materials Japan LLC Website: https://www.momentive.jp/content/momentive/jp/ja.html
- Lecture by Kiyoshi Ninomiya, “Tsukuru I (Career Development I)”, 6th Career Session, Sophia University Alumni Association, November 12.

